PCOS (Polycystic Ovary Syndrome) is a common hormonal disorder affecting millions of women worldwide, yet many remain undiagnosed. If you’re experiencing irregular periods, unexplained weight gain, or excessive hair growth, you might wonder if PCOS is the cause. Early detection is crucial, as PCOS can impact fertility, metabolism, and long-term health. In this article, we’ll break down the PCOS diagnosis tests, symptoms, and what to expect during the diagnostic process.
Recognizing the Symptoms: The First Step
Before testing, doctors assess symptoms to determine if further investigation is needed. Here’s a PCOS symptoms checklist to help identify potential warning signs:
- PCOS and irregular periods (missed, infrequent, or prolonged cycles)
- PCOS and hirsutism (excess hair growth on the face, chest, or back)
- PCOS and acne (persistent hormonal breakouts, especially along the jawline)
- PCOS and hair loss (thinning hair or male-pattern baldness)
- PCOS and weight gain (especially around the abdomen, linked to insulin resistance)
- PCOS and fertility issues (difficulty getting pregnant due to irregular ovulation)
If you experience several of these symptoms, your doctor may recommend tests to confirm the diagnosis.

PCOS Diagnostic Criteria: What Doctors Look For
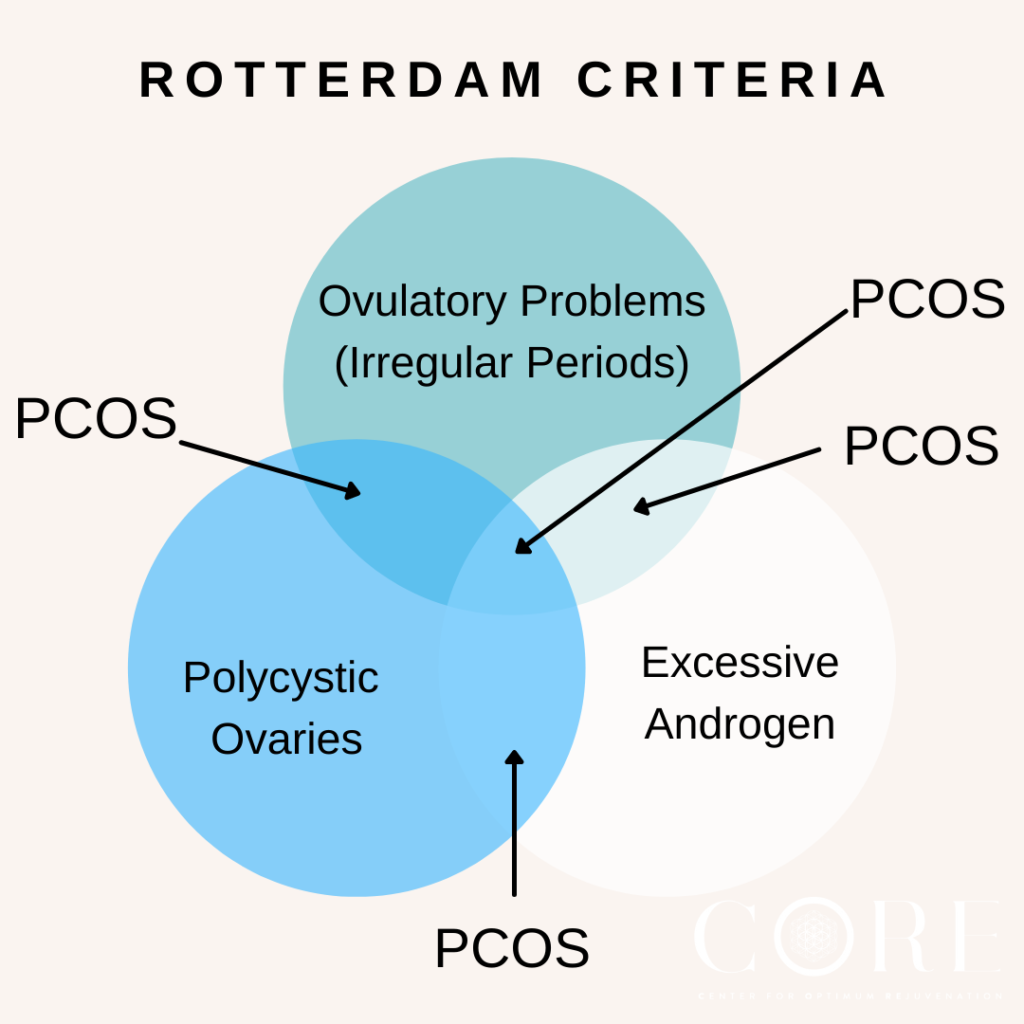
PCOS is diagnosed based on the Rotterdam Criteria, which requires at least two of the following three conditions:
- Irregular or absent ovulation (leading to menstrual irregularities)
- Elevated androgen levels (high PCOS and testosterone levels, causing symptoms like acne and hair growth)
- Polycystic ovaries on ultrasound (presence of multiple small cysts or follicles)
Meeting two of these criteria is enough for a diagnosis, but additional tests help rule out other conditions.
Key PCOS Diagnosis Tests
1. PCOS Blood Tests: Measuring Hormone Levels
Doctors often perform PCOS blood tests to assess various hormone levels:
- PCOS and LH/FSH ratio – An imbalance in these hormones can indicate ovulatory dysfunction.
- PCOS and AMH levels – Anti-Müllerian Hormone (AMH) is often elevated in women with PCOS, indicating a higher ovarian follicle count.
- PCOS and prolactin levels – High prolactin can mimic PCOS symptoms and must be ruled out.
- PCOS and thyroid function – Hypothyroidism shares symptoms with PCOS and should be tested.
- PCOS and insulin resistance – High insulin levels suggest metabolic issues often seen in PCOS.
- PCOS and testosterone levels – Elevated androgens confirm hyperandrogenism, a key PCOS marker.
2. PCOS Ultrasound Findings: Checking for Ovarian Cysts
A transvaginal ultrasound helps examine the ovaries for cysts or follicle abnormalities. PCOS and ovarian cysts are common, but not all women with PCOS have cysts, making hormone tests equally important.
PCOS and Metabolic Health: Additional Tests
Since PCOS affects metabolism, doctors may check for PCOS and metabolic syndrome, a cluster of conditions that increase heart disease risk. Tests may include:
- Blood sugar levels (to detect insulin resistance or diabetes)
- Cholesterol and triglyceride levels
- Blood pressure monitoring
What Happens After a PCOS Diagnosis?
If you’re diagnosed with PCOS, your doctor will guide you on management strategies, which may include lifestyle changes, medications, or hormone therapy. While there’s no cure, early intervention can help manage symptoms and prevent complications.
Final Thoughts
PCOS diagnosis involves evaluating symptoms, hormone levels, and ovarian health. If you suspect you have PCOS, consulting a healthcare provider is the first step toward effective management. The earlier you address the condition, the better your long-term health outcomes will be.
Also Read.