Heart disease is the leading cause of death in both men and women, yet women often receive delayed diagnoses and less aggressive treatment than men. The truth is, gender differences in heart disease treatment persist due to medical biases, lack of awareness, and biological differences. Women’s heart disease underdiagnosis continues to put lives at risk, making it essential to understand why this gap exists and how to address it.
1. Women’s Heart Disease Symptoms Are Often Overlooked
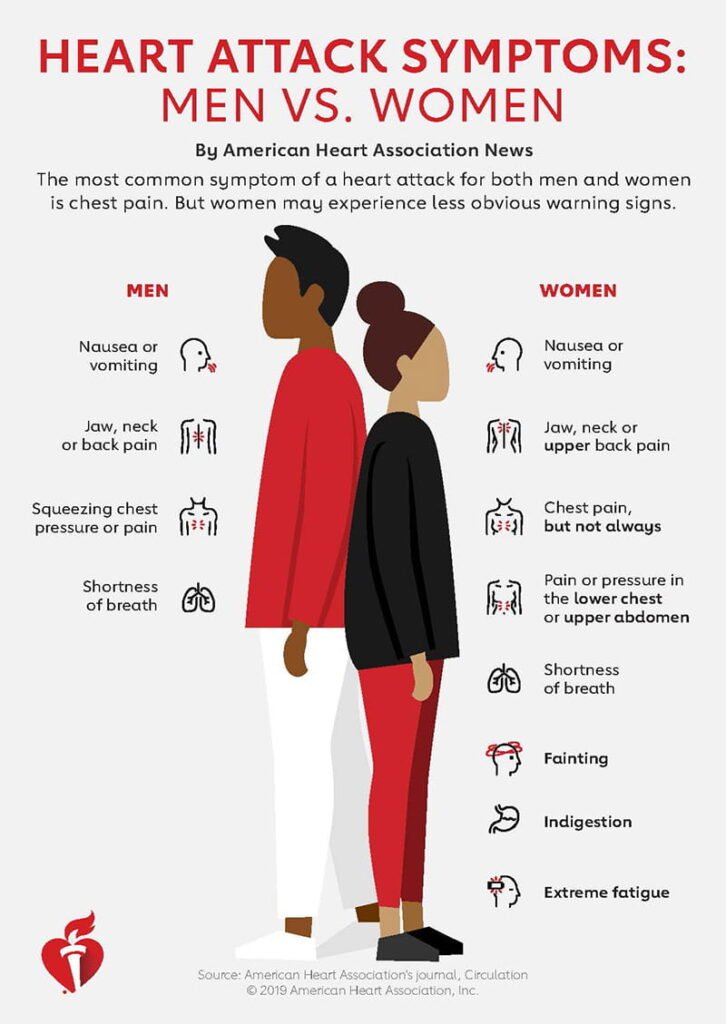
Heart disease symptoms in women vs. men can be vastly different. While men typically experience the classic crushing chest pain, women often report female heart attack symptoms like nausea, shortness of breath, or jaw pain. These atypical symptoms often lead to misdiagnosis or dismissal as anxiety or indigestion, delaying life-saving treatment.
2. Bias in Cardiac Care for Women
Medical research has historically focused on men, leading to bias in cardiac care for women. Many diagnostic tests and treatment protocols are based on male-centric studies, leaving gaps in knowledge about how heart disease presents in women. This bias results in women being less likely to receive timely interventions like angioplasty or bypass surgery.
3. Lack of Women in Cardiology Clinical Trials
Despite growing awareness, women in cardiology clinical trials remain underrepresented. This lack of female-specific research means that many treatments and medications are tested primarily on men, potentially leading to less effective care for women. More inclusive research is needed to improve outcomes for women.
4. Hormonal Impact on Women’s Heart Health
Hormones play a crucial role in cardiovascular health. The hormonal impact on women’s heart health is significant, particularly regarding estrogen’s protective effects before menopause. However, after menopause, women’s heart disease risk skyrockets, yet many treatment guidelines fail to account for these hormonal fluctuations.
5. Socioeconomic Factors in Women’s Heart Disease
Socioeconomic factors in women’s heart disease also contribute to disparities in treatment. Women often prioritize family responsibilities over their own health, delaying doctor visits. Additionally, financial barriers and limited access to specialized care prevent many women from receiving early diagnoses and necessary treatments.
6. Post-Menopausal Heart Disease Risk
Post-menopausal heart disease risk is another critical issue. As estrogen levels decline, women become more prone to high blood pressure, high cholesterol, and arterial plaque buildup. Unfortunately, many women are unaware of their heightened risk post-menopause, leading to missed opportunities for preventive care.
7. Lack of Awareness and Education
Many women and even healthcare professionals lack knowledge about heart disease risk factors unique to women. Women’s heart health awareness campaigns are growing, but there’s still a long way to go in educating both the public and the medical community about the warning signs and necessary lifestyle changes.
8. Gender-Specific Treatment Guidelines Are Lacking
Sex-specific cardiovascular treatment guidelines are needed to close the treatment gap. Standard heart disease protocols have been tailored to male physiology, often ignoring the unique aspects of female cardiovascular health. Developing and implementing female-specific guidelines could lead to more accurate diagnoses and effective treatments.
9. The Need for More Heart Disease Awareness Campaigns for Women
More heart disease awareness campaigns for women are essential to help bridge the knowledge gap. Public health initiatives should focus on educating women about their risks and symptoms while also encouraging healthcare providers to adopt a more gender-sensitive approach to heart disease diagnosis and treatment.
10. Improving Heart Disease Outcomes in Women
The ultimate goal is improving heart disease outcomes in women by increasing research, refining treatment guidelines, and ensuring equal access to quality care. Women must advocate for their heart health, push for second opinions when necessary, and take proactive steps to reduce their risk factors.
Final Thoughts
Women deserve the same quality of heart disease care as men, yet they often face delays in diagnosis and treatment due to biases, lack of research, and unique risk factors. Recognizing gender differences in treatment of heart disease and taking steps to close the gap can help save lives. By prioritizing women’s heart disease awareness, advocating for better research, and ensuring equal medical attention, we can work toward a future where every woman receives the heart care she needs and deserves.