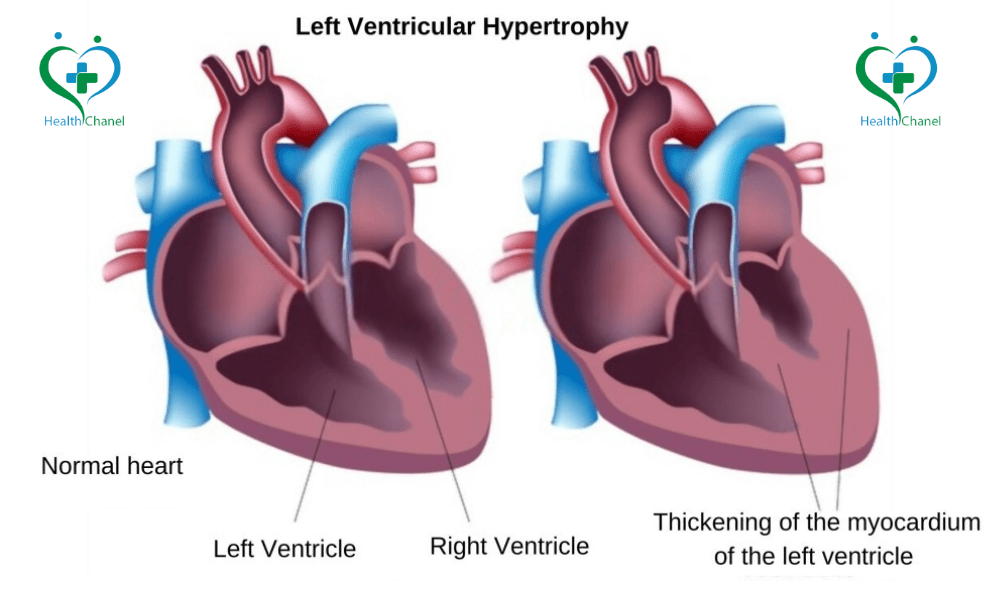
The heart hypertrophy definition refers to the thickening of the heart muscle, particularly the ventricles, due to excessive strain. In the case of Left Ventricular Hypertrophy, the thickening of the heart ventricle occurs in the left side of the heart, making it harder to pump blood effectively.Over time, untreated LVH can lead to heart failure, arrhythmias, or even sudden cardiac death. Conditions like high blood pressure, aortic regurgitation, and heart valve diseases can contribute to thickening of the heart ventricle.
What are Symptoms of Left Ventricular Hypertrophy?
LVH symptoms can vary. Some people experience no symptoms at all, while others may notice:
- Shortness of breath (especially during exertion)
- Chest pain or discomfort
- Dizziness or fainting
- Heart palpitations (rapid or irregular heartbeat)
- Fatigue or weakness
- Swelling in the legs or ankles (due to fluid retention)
If you have left ventricular hypertrophy with repolarization abnormality, you might also experience ECG changes that could signal more significant heart stress.
What are the Causes of Left Ventricular Hypertrophy?
Several factors can contribute to LVH and thickening of the heart ventricle:
- High blood pressure (hypertension) – The most common cause of LVH. Over time, the heart has to work harder to pump blood, leading to enlargement of the left ventricle.
- Aortic regurgitation – This condition forces the heart to pump extra blood, leading to ventricular hypertrophy.
- Aortic stenosis – A narrowed aortic valve increases resistance, making the heart work harder.
- Genetics – Some people inherit conditions that cause heart hypertrophy.
- Athlete’s heart – Intense exercise can lead to mild concentric LVH, which is usually harmless.
- Obesity and sleep apnea – Both conditions increase heart strain and can lead to probable left ventricular hypertrophy.
Diagnosis of LVH
LVH is often diagnosed through routine tests like:
- 12-lead ECG left ventricular hypertrophy – Electrical signals from the heart can indicate abnormal ECG left ventricular hypertrophy patterns.
- Echocardiogram – The most accurate test for identifying mild, moderate, or severe concentric left ventricular hypertrophy.
- MRI or CT scans – Used in some cases for more detailed imaging.
- LVH blood work – Blood tests can help rule out underlying conditions like kidney disease or hormonal disorders.
Treatment of Left Ventricular Hypertrophy
Lifestyle Changes
The first step in LVH treatment is reducing stress on the heart:
- Lower blood pressure – Controlling hypertension is key to ventricular hypertrophy treatment.
- Exercise regularly – Low-impact activities like walking and swimming help without overstraining the heart.
- Eat a heart-healthy diet – Focus on whole grains, lean proteins, and heart-friendly fats.
- Quit smoking and limit alcohol – Both can worsen enlarged left ventricle symptoms.
Medications for LVH Treatment
Doctors may prescribe:
- Blood pressure medications – Such as beta-blockers, ACE inhibitors, or calcium channel blockers.
- Diuretics – Help remove excess fluid and reduce heart strain.
- Medications for repolarization abnormalities – If you have left ventricular hypertrophy with repolarization abnormality, your doctor may prescribe specific drugs to regulate heart rhythms.
Surgical and Advanced Treatments
If medications aren’t enough, additional enlarged left ventricle treatment options include:
- Aortic valve replacement – If aortic stenosis is causing LVH.
- Pacemakers or defibrillators – If LVH with repolarization abnormality leads to dangerous arrhythmias.
- Myectomy – A surgical procedure to remove excess heart muscle in severe cases.
For more tips, Click here