Quick Navigation
What Is Endometriosis?
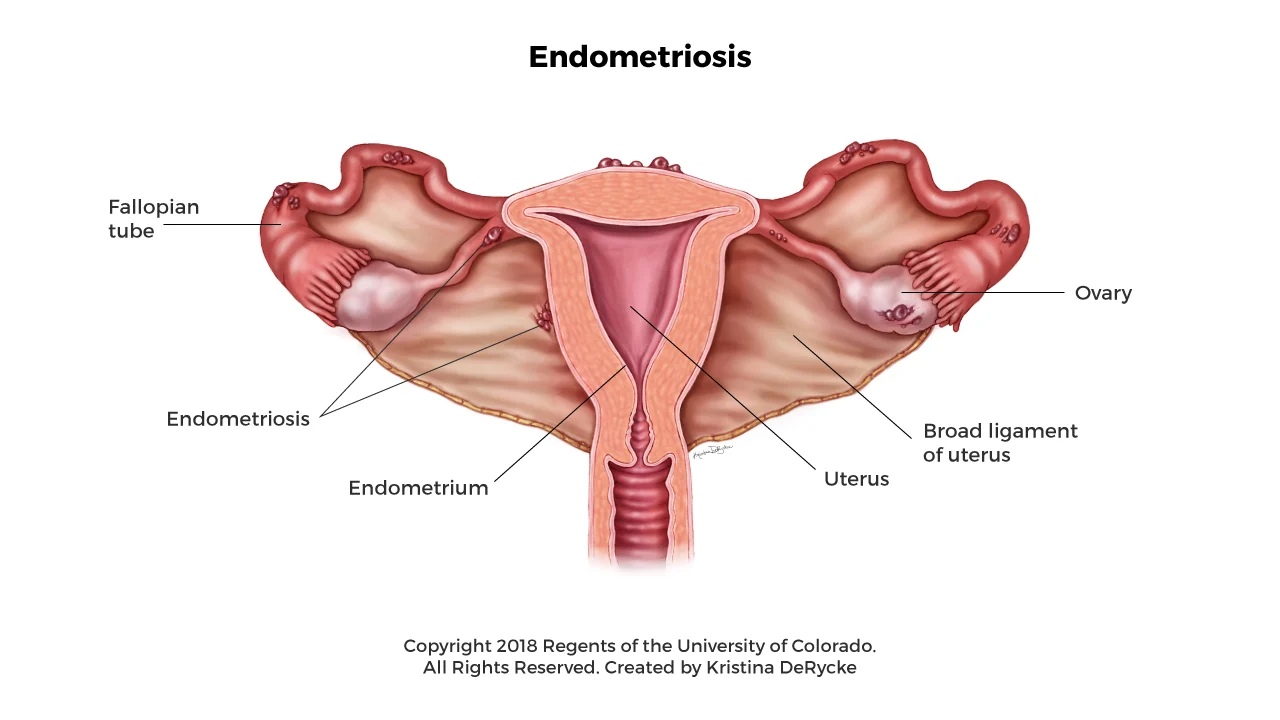
Endometriosis is a chronic condition where tissue similar to the lining of the uterus, called endometrium, starts growing outside the uterus. This misplaced tissue can attach to organs like the ovaries, fallopian tubes, bladder, and even the intestines. Although it behaves like regular uterine lining—thickening and breaking down with each menstrual cycle—it has nowhere to go, leading to inflammation, pain, and sometimes scar tissue.
It’s not just a “bad period.” Endometriosis can affect your day-to-day life, emotional health, and even your fertility.
Common Symptoms of Endometriosis
Symptoms can vary from person to person. Some people have severe pain, while others may not notice anything unusual. Here are the most common signs to look out for:
- Pelvic pain that often gets worse during menstruation
- Painful periods that interfere with daily activities
- Pain during or after sex
- Pain with bowel movements or urination, especially during periods
- Heavy menstrual bleeding or spotting between periods
- Fatigue and low energy
- Digestive issues like bloating, constipation, or diarrhea
- Difficulty getting pregnant
Keep in mind that having one or more of these symptoms doesn’t confirm endometriosis—but it’s worth talking to a healthcare provider if they’re impacting your quality of life.
What Causes Endometriosis?
The exact cause of endometriosis is still unknown, but several theories exist:
- Retrograde menstruation: This happens when menstrual blood flows backward into the pelvic cavity instead of out of the body.
- Immune system issues: Some experts believe the immune system may fail to remove misplaced endometrial cells.
- Genetics: If a close relative has endometriosis, your risk may be higher.
- Hormonal imbalance: Estrogen seems to promote the growth of endometrial-like tissue.
- Surgical spread: In rare cases, endometrial cells may be transferred to other areas during surgery, such as a C-section.
It’s likely that a mix of genetic, immune, and hormonal factors play a role in developing the condition.
How Is Endometriosis Diagnosed?
Diagnosis can be tricky because symptoms often mimic other conditions like IBS or ovarian cysts. A definitive diagnosis usually involves:
- Medical history and symptom discussion
- Pelvic exam to feel for abnormalities
- Ultrasound or MRI to check for cysts or tissue growths
- Laparoscopy—a minor surgical procedure that allows doctors to see inside the abdomen and confirm the presence of endometriosis
Early diagnosis is important, not just for managing pain, but also for protecting long-term reproductive health.
Treatment Options for Endometriosis
There’s no one-size-fits-all treatment, but the goal is to relieve symptoms and improve quality of life. Here are the main options:
Pain Management
Over-the-counter pain relievers like ibuprofen or naproxen can help reduce inflammation and ease menstrual cramps, but they may not be enough for everyone.
Hormonal Therapy
Hormone-based treatments aim to slow the growth of endometrial tissue. These include:
- Birth control pills or patches
- Progestin-only therapy
- GnRH agonists, which temporarily reduce estrogen production
- Hormonal IUDs
These treatments don’t cure endometriosis, but they can help manage the symptoms.
Surgery
For moderate to severe cases, surgery may be recommended to remove endometrial implants and scar tissue. Laparoscopic surgery is the most common method. Some people may require more extensive surgery if organs are affected.
Fertility Treatment
If endometriosis is affecting your ability to conceive, options like in vitro fertilization (IVF) or assisted reproductive technologies may be considered.
Lifestyle and Support
In addition to medical treatment, lifestyle changes can make a big difference:
- Anti-inflammatory diet rich in fruits, vegetables, and omega-3s
- Regular physical activity to ease pain and reduce stress
- Mind-body practices like yoga or meditation
- Support groups or therapy to help cope with the emotional toll
Can Endometriosis Be Cured?
There is currently no permanent cure for endometriosis, but many people are able to manage their symptoms effectively with the right treatment plan. Ongoing care, symptom tracking, and a supportive healthcare team can significantly improve quality of life.